Lupus in the Kidney: What are the dangers and what can be done about it?
As part of the awareness raising efforts for the just ended Lupus Awareness month, I would continue with a very important complication of that disease- Lupus nephritis. This is important as its one of the common causes of chronic kidney damage in young people.
What is Lupus Nephritis?
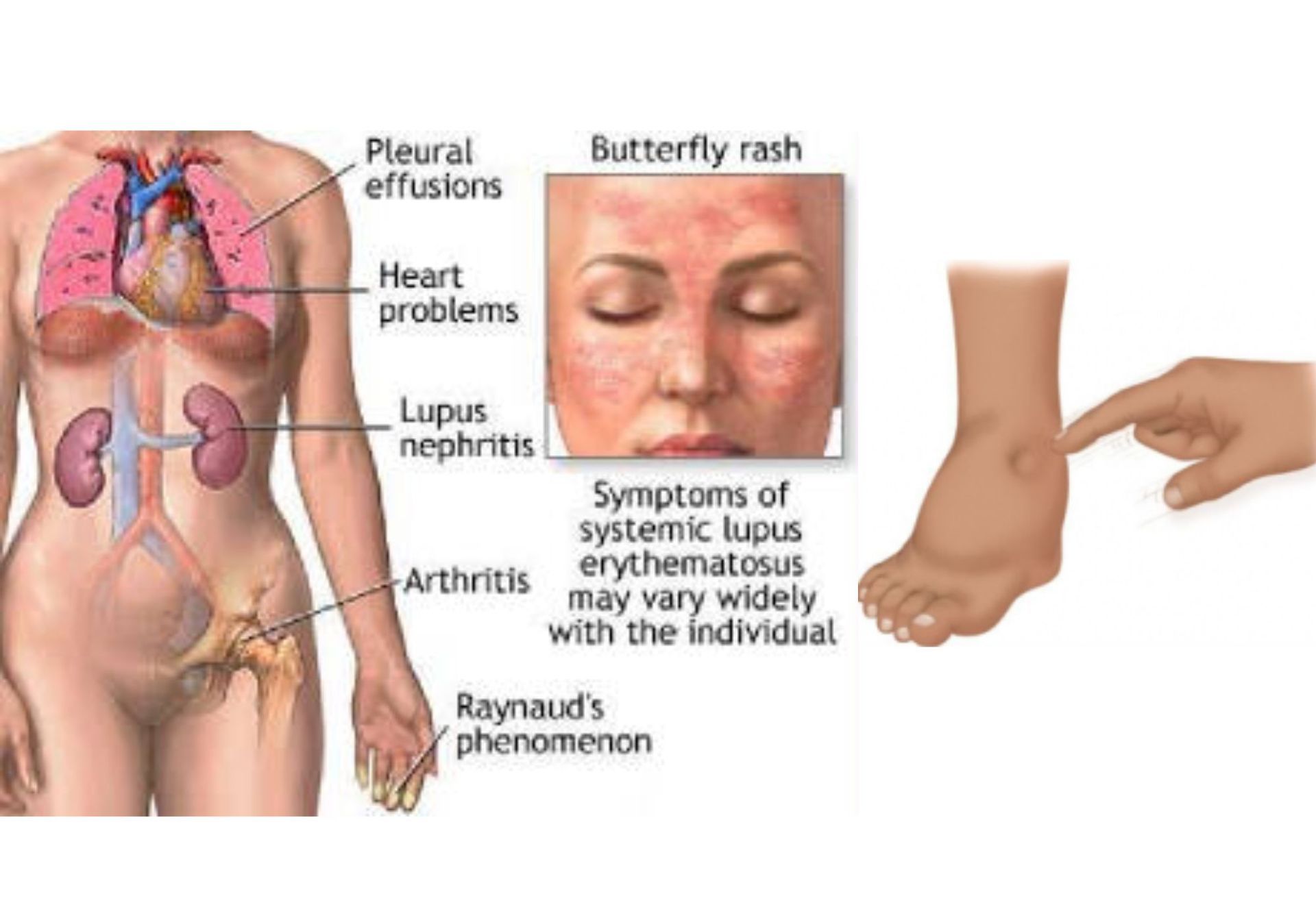
Systemic lupus erythematosus (SLE, or, more commonly “lupus”) is an illness in which the immune system begins attacking its own self. Normally, the immune system helps protect the body from infection or harmful materials. But in patients with an autoimmune disease, the immune system cannot tell the difference between harmful substances and healthy ones, resulting in the immune system attacking otherwise healthy cells and tissue.
Lupus nephritis is one of the most severe complications of lupus. It occurs when SLE causes the immune system to attack the kidneys. The kidneys are important for the body’s function. They remove waste from the blood, which would otherwise accumulate and cause illness and other metabolic disturbances. People with damaged kidneys might have to get regular dialysis. This is a procedure in which waste products in the blood is cleaned by a filtration machine. Some may require kidney transplantation.
Research suggests that about 50% of people with SLE suffer from lupus nephritis. SLE is most common in women ages 20 - 40. Anybody with lupus can potentially have kidney involvement, but people with lupus who have antibodies to double stranded DNA (anti-dsDNA) and low complement proteins ( particularly C3) and patients of African, South American or Asian descent have increased risk and should be watched more carefully for warning signs.
Symptoms
Lupus nephritis symptoms are similar to those of other kidney diseases. They include:
- dark urine
- blood in urine
- foamy, frothy urine
- having to urinate often at night
- puffy feet, ankles, and legs that gets progressively worse as the day goes along
- gaining weight
- high blood pressure
Blood Tests
Kidney function tests may show elevated levels of waste products, such as creatinine and urea.
24-Hour Urine protein Collection
This test measures the kidney’s ability selectively to filter wastes. It determines how much protein appears in urine over 24 hours.
Urine Tests
They identify levels of Protein, red blood cells, white blood cells and casts in the urine.
It is important to ascertain if the protein is from renal disease as some drugs that are commonly used in lupus such as ibuprofen or naproxen can cause reversible protein in the urine. Dehydration, excessive exercise, toxins, diabetes and many other conditions can also cause protein urine .
Ultrasound
This is done to look at the size and shape of the kidney and determine whether there is evidence of damage to the kidneys
Kidney Biopsy
Biopsies are the most accurate way to diagnose kidney disease. A long needle is passed through the back and into the kidney and a sample of kidney tissue is taken and analysed for signs and type of damage in the laboratory.
Often, protein in the urine is the first sign of lupus in the kidney. If no other cause is found for it and if the protein does not go away on rechecking it is very vital to get a kidney biopsy as soon as possible. This is because getting treated for lupus nephritis as soon as possible after it is noticed is very important, and without a proper diagnosis the wrong treatment could be given. Even within the spectrum of lupus, there are different forms of nephritis.
It is also essential to get a biopsy to ascertain if there is already kidney damage before treatment is initiated. This determines if there is chronic damage or active disease ad is rated on a scoring system called a chronicity scale. If there is already damage to the kidney, it is more difficult to get the best results with treatment. On the other hand, if there is no chronicity, it suggests that the nephritis was caught early and then chances of success with treatment are very good.
Treatment:
There is no cure for lupus nephritis. The goal of treatment is to keep the problem from getting worse and stopping kidney damage early.
Treatment modalities include:
- minimizing intake of protein and salt
- lowering cholesterol levels
- taking blood pressure medication
- using steroids to reduce immune system damage to the kidneys.
- other medications that suppress the immune system, such as cyclophosphamide, mycophenolate mofetil, or azathioprine and newer medication like Rituximab.
Complications
The most serious complication associated with lupus nephritis is kidney failure. People with kidney failure will need either dialysis or a kidney transplant. Dialysis may be needed to control symptoms of kidney failure, sometimes for only a while.
Hope for the future
Currently, there are new diagnostic tests being developed in the hopes that in future, kidney biopsies can be avoided, and accurate diagnosis and treatments might be started even earlier. There are also some potentially powerful new treatments in development. There is even some hope that some new drugs that are being made to reduce scarring in tissues might in the future be used to reverse chronicity that has already occurred in the kidney.
In the meantime, the key to dealing with lupus kidney disease effectively is knowing if you might be at higher risk, getting regular monitoring, early diagnosis and treatment.










